
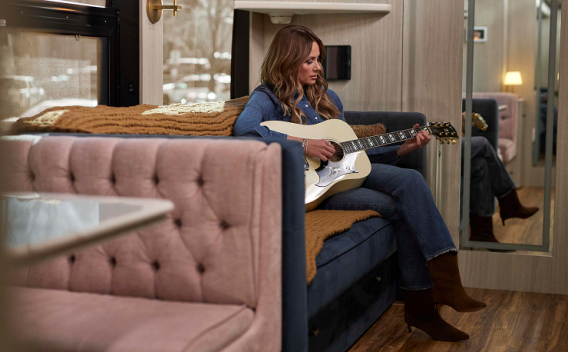
Carly Pearce, Grammy-winning country music singer/songwriter, living with recurrent pericarditis
Patient stories
Dive into the real stories of patients with recurrent pericarditis—from students to superstars. Recurrent pericarditis can affect anyone and everyone has useful insights to share.
Hear from Carly
Carly Pearce, country music singer/songwriter living with recurrent pericarditis, shares how it first threatened to disrupt her music career—and how she keeps going.
Watch Henrik’s video
Henrik Lundqvist, NHL Hall-of-Famer living with recurrent pericarditis, shares what it was like to first learn he had the condition—and how he’s forged ahead to keep living life.

Watch Jill’s story
Jill, a mom and high school superintendent, who lives with recurrent pericarditis and shares how she is fighting both flares and a lack of readily available pericarditis information.

Hear from Joao
Joao, a medical student who is living with recurrent pericarditis gives us his take on diagnosis and treatment.

Learn from a pericarditis specialist
Dr. Jonathan Salik, a cardiologist in Boston, Massachusetts, who specializes in recurrent pericarditis, shares some expert insights for managing recurrent pericarditis.

Last updated: 04/30/25
The content on this page has been written and approved by Kiniksa Pharmaceuticals.