
Carly Pearce, Grammy-winning country music singer/songwriter, living with recurrent pericarditis
Acute pericarditis flare:
An episode of pericarditis which may present with symptoms such as sharp chest pain.
First episode of pericarditis:
The first flare, which often goes away after a few weeks either on its own or after treatment.
Recurrent pericarditis (RP):
When another flare happens more than 4 weeks after first flare goes away. Recurrent pericarditis can be a chronic disease, meaning that it may last for many years.
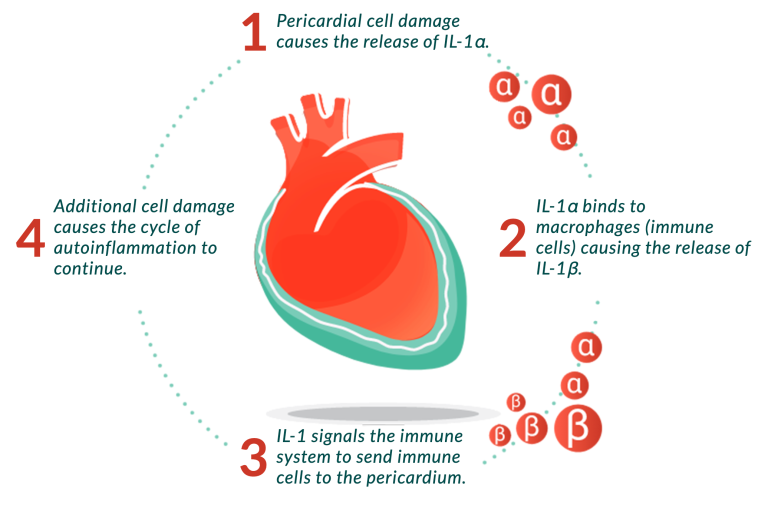
Recurrent pericarditis is an autoinflammatory disease, meaning that the flares are caused by the body's immune system attacking the pericardium. Each attack causes inflammation that leads to an ongoing cycle of inflammation.
Quote from Dr. Jonathan Salik
"Research shows that the average patient with recurrent pericarditis might experience symptoms for three to four years and up to a quarter of patients might experience symptoms for eight years or longer."
How do you know a flare is beginning?
Hear from Joao
A medical student who is living with recurrent pericarditis gives us his take on diagnosis and treatment issues.

With each recurrent pericarditis flare, the risk of having another flare increases
In a study of 7502 patients with pericarditis:
With each flare, the time between flares decreases.
Did you know?
Recurrent pericarditis can be so painful that it is often mistaken for a heart attack. Flares can often lead to hospital stays and emergency room visits.
Recurrent pericarditis by the numbers
Up to 1 in 3 people
with a first episode of pericarditis will experience recurrent pericarditis within 18 months of their first flare.

There are approximately 40,000 people
with recurrent pericarditis in the United States who seek care annually.

There are an estimated 20,000
new cases of recurrent pericarditis in the United States each year.

Recurrent pericarditis can impact anyone, including men, women, age groups, racial groups, and economic levels.
The cycle of autoinflammation in recurrent pericarditis
There are even more types of pericarditis than first episode of pericarditis and recurrent pericarditis.
Did you know?
Episodes of pericarditis are commonly referred to as “flares.”
Last updated: 04/30/25
The content on this page has been written and approved by Kiniksa Pharmaceuticals.